|
Indigent are most likely to get sick or injured
but rarely have insurance
by Will Sands
 |
| An ambulance waits for its next
assignment outside Mercy Medical Center on Tuesday. Many people
without access to health care or without insurance end up
in Mercy’s emergency room as a last resort./Photo by
Todd Newcomer. |
Two years ago, Bruce Deile was diagnosed with Lyme disease during
a stint in Santa Rosa, Calif. At the time, he was given a three-week
course of antibiotics to treat the disease, but according to Deile,
“it didn’t seem to kill the infection.” The
38-year-old said that the disease is currently inflaming his brain
and spinal cord and, if left untreated, could paralyze or kill
him.
“After being diagnosed, I traveled to seven different states
and can’t get the intravenous antibiotics that the National
Institutes of Health say bring full recovery,” Deile noted.
Deile said he believes he can’t get the medicine in large
part because he is homeless, has been for the last six years and
can’t afford the expensive treatment. Deile’s quest
for health care arrived in Durango two months ago, joining numerous
others without housing or health insurance who face a steep path
to recovery. This picture may worsen before it improves.
John Gamble, Volunteers of America division director and supervisor
of the Durango Community Shelter and the Southwest Safehouse,
said that the homeless population faces a doubly hard health picture.
First, they are often more susceptible to health problems.
“There’s a vulnerability in the sense that you’re
often living in the street, your nutrition is less favorable and
in the case of some homeless people, your lifestyle choices are
less favorable,” Gamble said. “There are people who
every winter live in stick and canvas lean-tos in the hills, and
those people are vulnerable.”
Second, these people who are most likely to get sick or encounter
health problems are also least likely to have health insurance
coverage.
“The lack of access to health care for low income and homeless
people is really a reflection of a growing national problem,”
Gamble said. “Durango is full of employers who don’t
supply health insurance. At how many hundreds of dollars a month
does it become feasible for a homeless person to even think about
having health coverage?”
The net effect is a situation that spirals downward to a disastrous
end, according to Gamble and Teresa DeGuelle, program manager
for the VOA Community Shelter.
“One of the biggest issues is that these people may fall
ill, but they don’t get treated and it spirals into a more
serious condition,” DeGuelle said.
Gamble added, “You end up having folks who may delay access
to health care for one reason or another and they’ll wait
until they get sick and go to the emergency room. And we all know
that the emergency room is the most expensive health care you
can pay for.”
And while the common perception of the homeless person is of
a male drifter with a substance-abuse problem, Gamble said that
Durango’s homeless population does not fit the stereotype.
Instead he pointed to a large number of local individuals and
families who have fallen on hard times. Deile also contrasts the
stereotype and is proud of the fact that he has been clean and
sober since 1985, long before he became homeless.
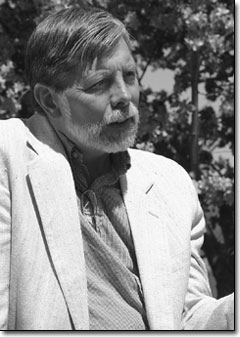 |
John Gamble, of the Volunteers of America
Community Shelter and the Southwest Safehouse, talks about
the state of health care for the homeless. He said problems
with health care access also impact low- and middle-income
segments of the local population./Photo by Todd Newcomer. |
Gamble also commented that 40 percent of Community Shelter residents
are women and children, and that all of the residents of the Southwest
Safehouse are women and children. With these factors in mind,
he said that the lack of health-care access is particularly upsetting.
“We have a large number of children in this community with
no access to health care and that’s so wrong,” Gamble
said.
He added that health care access may be visibly difficult for
the local homeless population but also impacts low- and middle-income
segments of the local population. “I think it’s important
to recognize that this is a problem demonstrated in the homeless
community, but experienced by working families all over this city,
state and nation,” he said.
Despite an apparently bleak health-care future for these segments
of the local population, Gamble said that Durango does have an
upside. Mercy Medical Center’s open-door policy does offer
some hope.
“I can’t say that I’m aware of people who are
homeless and dying on the streets,” he said. “The
medical safety net in this community is Mercy. When all else fails,
they will pick up the pieces.”
David Bruzzese, spokesman for 4 Mercy Medical Center, commented,
“We’re the safety net for everyone, homeless or not.
If you can’t afford health insurance, it doesn’t matter
to us. We serve everyone regardless of their ability to pay.”
To this end, Mercy wrote off $3.9 million in unreimbursed Medicaid
and Indigent Care costs during the 2003 fiscal year.
“What distinguishes us is, we are open 24 hours a day and
care for everyone who comes through our doors regardless of their
ability to pay,” Bruzzese said.
The one caveat is that the care is only for people who come through
the emergency room doors with an immediate life-threatening condition;
there are no provisions at Mercy for indigent primary care. Three
weeks ago, Diele went to the Mercy emergency room seeking treatment
for complications from his Lyme disease. At that time, he did
not receive the intravenous antibiotics he says are necessary.
“I’ve gone to the emergency room most recently here
in Durango because of the neurological manifestation of the disease,”
he said. “I’m told that Lyme disease is a chronic
condition and that they’re not obligated to treat it because
it isn’t acute. I’ve been told I’m only qualified
for the cheap treatment.”
Bruzzese said that Mercy is not a primary care provider and that
often makes the emergency room the only option for people like
Deile. “We don’t employ primary care physicians, so
for most people who can’t afford primary care, the emergency
room becomes their last option,” he said.
Still, Bruzzese said that Mercy and its employees deserve credit
for the service they provide to those in need. “It’s
not only Mercy as an organization that supports the community,
it’s the care providers that make sacrifices and help people
heal and repair their bodies and improve their well being and
condition in life,” he said.
Although Gamble wholeheartedly agreed that Mercy is providing
an invaluable service to the community at large, he said that
more is needed. One cooperative step between the VOA and Mercy
that has been successful is the Community Shelter’s “Medical
Respite Bed” program, he said. Over the years, the shelter
has helped homeless people with everything from broken bones to
Lou Gehrig’s disease recover. In 2002, the program saw more
than 500 user nights. Last year, it had more than 250 nights.
“Mercy realistically can’t discharge a seriously
ill person into a situation where there is not care,” Gamble
said noting that the “Medical Respite Bed” helps fill
that void.
“It costs us about $25 a night to have someone in that
bed,” Gamble continued. “I don’t think anyone
can get out of the door of the hospital for less than $1,000 a
night. With this bed, we’ve been able to save enormous amounts
of money for the community. It’s been a very successful
partnership.”
As a further solution to the problem, DeGuelle said it would
be nice to see the return of a community clinic to Durango. “I
think a community clinic that was on a straight sliding scale
would be very beneficial for everyone here,” she said.
And Gamble said that primary care providers could also help lend
a hand to local people in need. “We realize that you can’t
go to the well too often,” he said. “But if a medical
office could see one person a month or some other modest level
of commitment, that could help to address the problem.”
Still, more global solutions are required not just for the homeless
but for everyone who struggles with the expense of health care,
said Gamble. “The final sad commentary is that the wealthiest
nation in the country spends more than any other country in the
world on health care and yet we have the worst access to health
care,” he said. “There is something evidently wrong
with this picture.”
As evidence, Deile said he is seeing his search for health care
go nowhere. He considered travelling to the East Coast in hopes
of finding the remedy, but travel is becoming harder. Instead
he is resolving to accept the worst-case scenario. “It’s
gone on so long,” he concluded. “It seems like it’s
the reality that treatment is not going to be available.”
|

